Contents
- 1 The Current State of AI in Healthcare
- 2 The Optimistic Vision: Transformative Benefits of AI in Medicine
- 3 The Pessimistic
Perspective: Risks and Concerns
- 3.1 Algorithmic Bias and Health Inequities
- 3.2 Privacy Violations and Data Security Risks
- 3.3 The Black Box Problem and Accountability
- 3.4 Safety Concerns and Medical Errors
- 3.5 Erosion of the Human Element in Healthcare
- 3.6 Regulatory Gaps and Governance Challenges
- 3.7 Economic Disruption and Job Displacement
- 4 Finding Balance: A Path Forward
- 5 Conclusion: Embracing Complexity
AI-powered medical technology is transforming the future of healthcare delivery
The intersection of artificial intelligence and healthcare represents
one of the most transformative developments in modern medicine. As we
navigate through 2025, AI technologies are no longer experimental
curiosities confined to research laboratories—they have become integral
components of healthcare systems worldwide, fundamentally reshaping how
we diagnose diseases, treat patients, and manage health outcomes. This
revolution brings with it both extraordinary promise and significant
challenges that demand our careful attention.
The Current State of AI
in Healthcare
The healthcare industry has witnessed an unprecedented surge in AI
adoption over recent years. By August 2024, the U.S. Food and Drug
Administration had authorized approximately 950 medical devices
incorporating artificial intelligence or machine learning capabilities,
with the majority focused on disease detection and diagnosis,
particularly in radiology. This explosive growth reflects a broader
trend: AI-related healthcare publications have skyrocketed from just 158
in 2014 to 731 in 2024, demonstrating the field’s rapid maturation.
Today’s AI applications in healthcare span an impressive range of
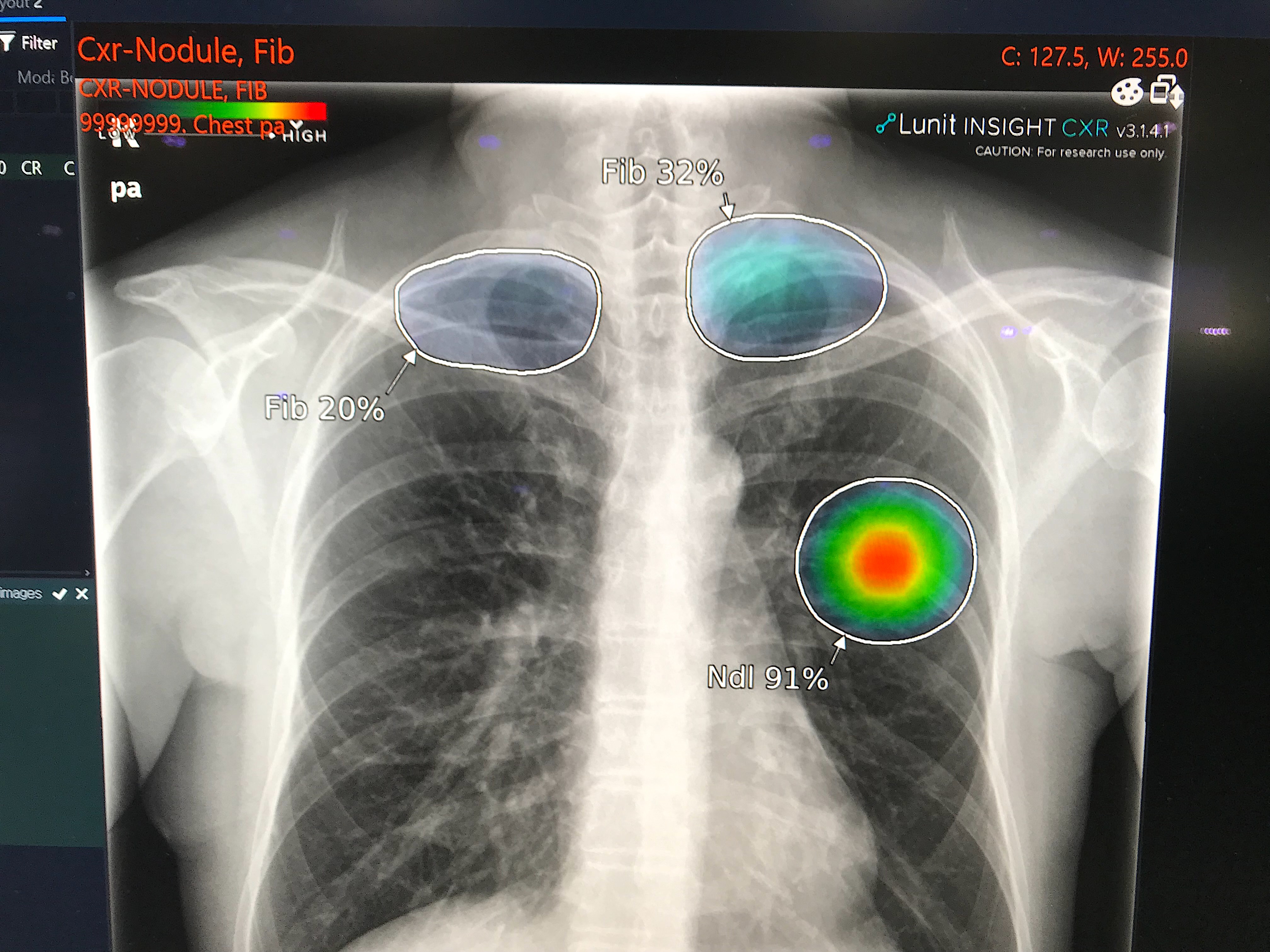
capabilities. Machine learning algorithms are achieving remarkable
accuracy in medical imaging, with some systems detecting lung nodules
with 94% accuracy and identifying breast cancer with 90%
sensitivity—often matching or surpassing human radiologists. These
systems leverage sophisticated deep learning architectures, particularly
convolutional neural networks (CNNs), to analyze medical images and
identify patterns that might escape human observation.

diagnostic accuracy across multiple medical specialties
Beyond diagnostics, AI is revolutionizing clinical workflows through
ambient listening technology that automates clinical documentation,
retrieval-augmented generation (RAG) systems that enable accurate data
querying, and intelligent clinical coding that reduces administrative
burdens. Virtual health assistants powered by AI are handling patient
triage, answering routine inquiries, and managing appointment
scheduling, freeing healthcare professionals to focus on complex medical
decision-making.
The technology has also made significant inroads in drug discovery,
where AI accelerates the identification of new therapeutic targets and
optimizes clinical trial design. Predictive analytics platforms are
analyzing electronic health records to anticipate disease progression,
identify patients at risk for complications, and recommend personalized
treatment strategies. In surgical settings, AI-assisted robotic systems
are enabling unprecedented precision in complex procedures, from
neurosurgery to dental operations.
The
Optimistic Vision: Transformative Benefits of AI in Medicine
The potential benefits of AI in healthcare are nothing short of
revolutionary, promising to address some of medicine’s most persistent
challenges while opening new frontiers in patient care.
Enhanced
Diagnostic Accuracy and Early Detection
Perhaps AI’s most celebrated contribution lies in its diagnostic
capabilities. AI systems can process vast amounts of medical data—from
imaging studies to genomic sequences to clinical histories—identifying
subtle patterns and correlations that might elude even experienced
clinicians. This capability is particularly valuable in early disease
detection, where AI algorithms can spot precancerous lesions, identify
cardiovascular risks from retinal scans, and detect diabetic retinopathy
before symptoms appear.
Recent breakthroughs include AI models that can predict genetic risks
for hereditary diseases, analyze pathology slides for cancer detection
with remarkable precision, and even forecast individual disease risks
for over 1,000 conditions—akin to weather forecasting for health. These
predictive capabilities enable proactive interventions that can prevent
disease progression or catch conditions at their most treatable
stages.
Personalized and Precision
Medicine
AI is ushering in an era of truly personalized healthcare. By
integrating multimodal data—genomic information, medical imaging,
clinical records, lifestyle factors, and real-time monitoring from
wearable devices—AI systems can tailor treatment plans to individual
patients with unprecedented specificity. This approach optimizes drug
selection and dosing, predicts treatment responses, and identifies the
most effective interventions based on a patient’s unique biological and
clinical profile.
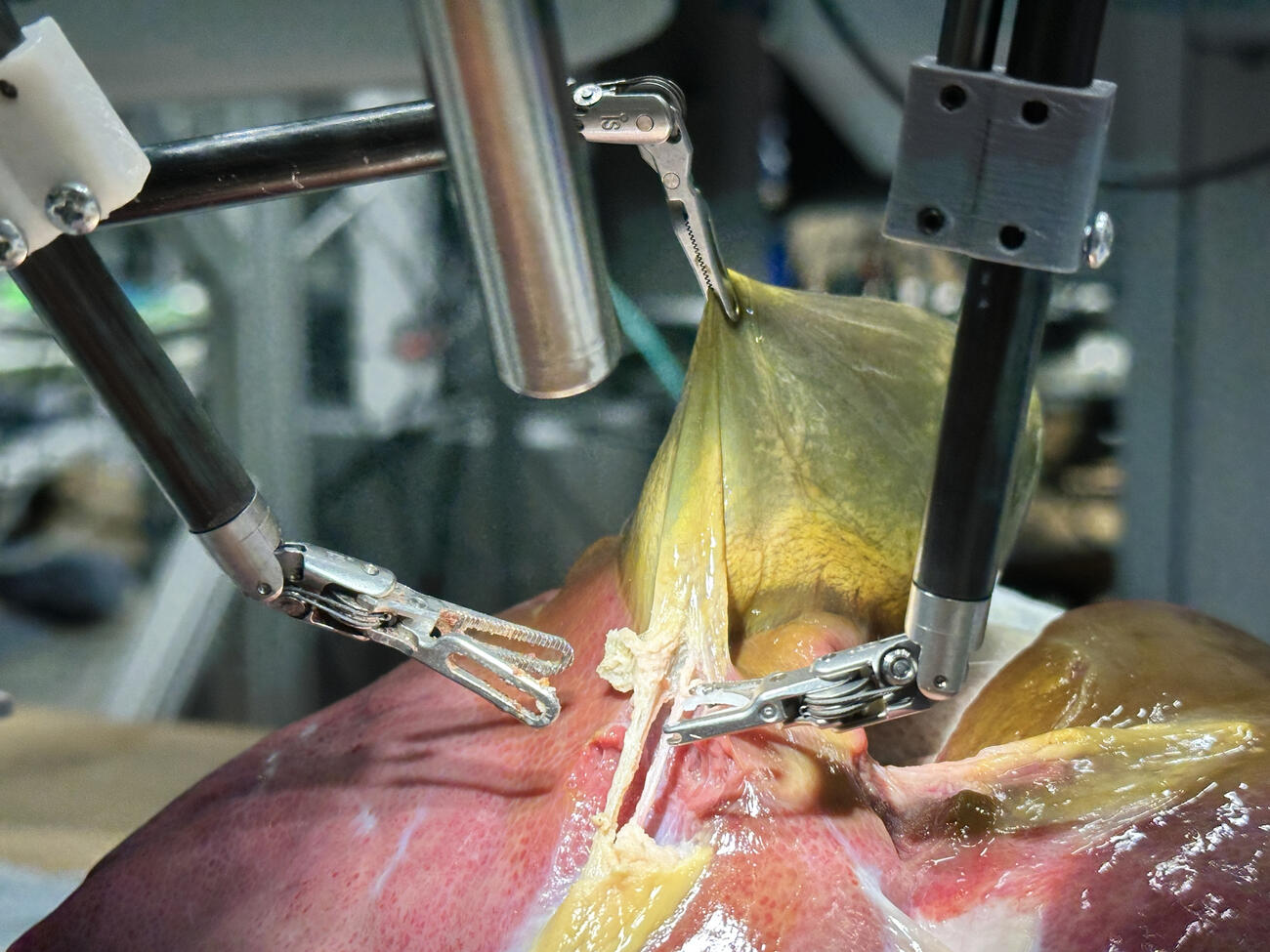
enabling precision in complex surgical procedures
In oncology, AI analyzes tumor characteristics to recommend targeted
therapies. In cardiology, it predicts which patients will benefit most
from specific interventions. In chronic disease management, AI-powered
platforms continuously monitor patient data, adjusting treatment
recommendations in real-time to optimize outcomes while minimizing side
effects.
Operational
Efficiency and Cost Reduction
The economic impact of AI in healthcare extends far beyond improved
clinical outcomes. By automating routine tasks—from documentation and
billing to lab result interpretation and appointment scheduling—AI
dramatically reduces administrative overhead that currently consumes up
to 30% of healthcare spending in many systems. This efficiency
translates directly into cost savings that can make healthcare more
accessible and affordable.
AI-driven workflow optimization helps hospitals manage patient
throughput more effectively, reducing wait times and improving resource
allocation. Predictive analytics identify patients at high risk for
readmission, enabling targeted interventions that prevent costly
emergency department visits. In clinical trials, AI accelerates patient
recruitment and monitors safety signals, potentially reducing drug
development costs by billions of dollars.
Democratizing Healthcare
Access
Perhaps most profoundly, AI has the potential to democratize access
to high-quality healthcare. Telemedicine platforms enhanced with AI
diagnostic tools can bring specialist-level expertise to remote and
underserved communities. AI-powered triage systems help patients
navigate complex healthcare systems, directing them to appropriate care
levels and reducing unnecessary emergency department visits.
Virtual health assistants provide 24/7 support for medication
management, symptom checking, and health education, empowering patients
to take active roles in their care. For healthcare systems struggling
with physician shortages, AI augments human capabilities, enabling
smaller teams to serve larger populations without compromising care
quality.
Advancing Medical
Research and Innovation
AI is accelerating the pace of medical discovery in ways previously
unimaginable. Machine learning algorithms can analyze millions of
research papers, clinical trials, and patient records to identify
promising research directions and generate new hypotheses. In drug
discovery, AI screens billions of molecular compounds to identify
potential therapeutics, a process that once took years but now occurs in
months or weeks.
The technology is also revealing new insights into disease mechanisms
by identifying patterns in complex biological data that human
researchers might never detect. These discoveries are opening new
avenues for treatment and prevention, potentially leading to
breakthroughs in conditions that have long resisted medical
intervention.
The Pessimistic
Perspective: Risks and Concerns
While AI’s potential in healthcare is undeniable, its implementation
raises serious concerns that cannot be dismissed or minimized. These
challenges span technical, ethical, social, and regulatory domains, each
presenting obstacles that could undermine AI’s benefits or even cause
harm if not properly addressed.

important questions about privacy and security
Algorithmic Bias and
Health Inequities
One of the most troubling concerns surrounding AI in healthcare is
the potential for algorithmic bias to perpetuate or even exacerbate
existing health disparities. AI systems learn from historical data, and
if that data reflects societal biases or underrepresents certain
populations, the resulting algorithms will inherit and amplify those
biases.
Studies have documented numerous instances where AI diagnostic tools
perform poorly on underrepresented demographic groups—women, racial
minorities, and patients from lower socioeconomic backgrounds. An AI
system trained primarily on data from one population may misdiagnose
conditions in others, leading to delayed treatment or inappropriate
interventions. This risk is particularly acute in conditions that
present differently across demographic groups or in populations that
have historically received inadequate healthcare.
The consequences of biased AI extend beyond individual misdiagnoses.
If AI-driven resource allocation systems are trained on biased data,
they may systematically direct resources away from already underserved
communities, widening health equity gaps. Without careful attention to
data diversity and algorithmic fairness, AI could become a tool that
reinforces rather than reduces healthcare inequalities.
Privacy Violations
and Data Security Risks
AI’s hunger for data creates profound privacy concerns. Healthcare AI
systems require vast amounts of sensitive personal information—medical
histories, genetic data, lifestyle information, and real-time health
monitoring data. This concentration of sensitive data creates attractive
targets for cyberattacks and raises questions about who controls this
information and how it might be used.
Current privacy frameworks like GDPR and HIPAA, while important, were
designed for an earlier era and struggle to address AI-specific
challenges. Advanced algorithms can potentially re-identify supposedly
anonymized data, undermining privacy protections. The commercial
incentives surrounding health data—from pharmaceutical companies to
insurance providers to technology firms—create pressures that may not
align with patient interests.
Data breaches in healthcare can have devastating consequences beyond
financial loss. Exposed health information can lead to discrimination in
employment, insurance, and social contexts. The permanent nature of
genetic data means that breaches can affect not just individuals but
their families and future generations. As AI systems become more
sophisticated and data sharing becomes more common, these risks
multiply.
The Black Box Problem
and Accountability
Many AI systems, particularly those using deep learning, operate as
“black boxes”—their decision-making processes are opaque even to their
creators. When an AI system recommends a diagnosis or treatment,
clinicians and patients often cannot understand the reasoning behind
that recommendation. This opacity creates serious problems for medical
practice, which traditionally relies on transparent reasoning and the
ability to explain decisions to patients.
transparency and accountability in medical decision-making
The black box problem becomes particularly acute when AI makes
errors. Recent research from the National Institutes of Health found
that AI models can make mistakes in explaining medical images even when
reaching correct diagnoses, highlighting the disconnect between AI’s
outputs and its reasoning. When an AI-assisted diagnosis proves wrong,
determining accountability becomes nearly impossible. Is the AI
developer responsible? The healthcare provider who relied on the AI? The
institution that deployed the system?
This lack of transparency erodes trust—both among healthcare
providers who may be reluctant to rely on systems they don’t understand,
and among patients who may feel their care is being determined by
inscrutable algorithms. It also complicates the informed consent
process, as patients cannot truly understand the risks and benefits of
AI-assisted care when the systems themselves are opaque.
Safety Concerns and Medical
Errors
While AI promises to reduce medical errors, it also introduces new
categories of risk. AI systems can fail in unexpected ways, producing
confident but incorrect recommendations that may mislead clinicians. The
phenomenon of “automation bias”—the tendency to over-rely on automated
systems—means that healthcare providers might accept AI recommendations
without sufficient critical evaluation, particularly when workload
pressures are high.
AI systems trained on one population or in one clinical setting may
perform poorly when deployed elsewhere, a problem known as
“overfitting.” A diagnostic algorithm that works well in a
well-resourced academic medical center might fail catastrophically in a
rural clinic with different patient populations and equipment. These
failures may not be immediately apparent, potentially causing harm
before they’re detected and corrected.
The rapid pace of AI development also creates safety challenges.
Unlike traditional medical devices that undergo extensive testing before
deployment, AI systems can be updated continuously, potentially
introducing new bugs or behaviors without adequate validation. The lack
of standardized testing protocols and post-market surveillance for AI
systems means that problems may go undetected until significant harm has
occurred.
Erosion of the Human
Element in Healthcare
Healthcare is fundamentally a human endeavor, built on relationships,
empathy, and trust between patients and providers. The increasing role
of AI raises concerns about the dehumanization of medicine. When
algorithms mediate the patient-provider relationship, there’s a risk
that the compassionate, holistic aspects of care—understanding patients’
fears, values, and life circumstances—may be diminished.
Clinicians report concerns that excessive reliance on AI could lead
to deskilling, where healthcare providers lose the ability to make
independent clinical judgments. Medical students trained in an
AI-saturated environment might never develop the pattern recognition and
intuitive reasoning that comes from extensive clinical experience. This
dependency could prove catastrophic if AI systems fail or are
unavailable.
For patients, particularly those dealing with serious illness or
end-of-life decisions, the presence of AI in medical decision-making can
feel alienating. The knowledge that an algorithm is influencing their
care may undermine the therapeutic relationship and reduce patient
agency in their own healthcare decisions.
Regulatory Gaps and
Governance Challenges
The regulatory landscape for AI in healthcare is fragmented and
struggling to keep pace with technological advancement. Different
jurisdictions have different standards, creating confusion and
potentially allowing unsafe systems to reach patients. Many AI systems,
particularly those developed in-house by healthcare institutions, may
evade regulatory oversight entirely.
Current regulations often fail to address AI-specific challenges like
algorithmic bias, continuous learning systems that change over time, and
the use of AI in clinical decision support versus autonomous
decision-making. The lack of clear liability frameworks means that when
AI-related harm occurs, victims may have no clear path to compensation
or justice.
International coordination on AI governance remains weak, despite the
global nature of both AI development and healthcare challenges. Without
harmonized standards and robust oversight mechanisms, the risks of AI in
healthcare may outweigh its benefits, particularly for vulnerable
populations.
Economic Disruption
and Job Displacement
The efficiency gains from AI come with a human cost. Automation of
administrative tasks, diagnostic procedures, and even some aspects of
clinical care threatens jobs across the healthcare sector. Radiologists,
pathologists, medical coders, and administrative staff face potential
displacement as AI systems take over tasks they once performed.
While proponents argue that AI will augment rather than replace
healthcare workers, the reality may be more complex. Economic pressures
on healthcare systems create incentives to reduce labor costs, and AI
provides a means to do so. The resulting job losses could be
particularly severe in already economically disadvantaged communities,
exacerbating social inequalities.
Moreover, the concentration of AI development in wealthy nations and
large technology companies raises concerns about global health equity.
If AI-driven healthcare becomes the standard in high-income countries
while remaining inaccessible elsewhere, the global health divide could
widen dramatically.
Finding Balance: A Path
Forward
The future of AI in healthcare need not be a choice between
uncritical enthusiasm and paralyzing fear. Instead, we must chart a
middle course that maximizes benefits while actively mitigating risks
through thoughtful governance, ethical frameworks, and ongoing
vigilance.
Establishing Robust
Ethical Frameworks
Healthcare AI must be developed and deployed within clear ethical
frameworks that prioritize patient welfare, equity, and human dignity.
These frameworks should mandate transparency in AI decision-making,
require diverse representation in training data, and establish clear
lines of accountability when systems fail. Ethical review boards should
evaluate AI systems before deployment, with ongoing monitoring to detect
emerging problems.
Informed consent processes must evolve to address AI-specific
considerations, ensuring patients understand when and how AI influences
their care and preserving their right to opt out of AI-assisted
treatment. Healthcare providers need training not just in using AI tools
but in critically evaluating their recommendations and maintaining their
independent clinical judgment.
Strengthening Regulatory
Oversight
Regulatory frameworks must adapt to AI’s unique challenges. This
requires international coordination to establish harmonized standards,
mandatory post-market surveillance to detect problems after deployment,
and clear liability rules that protect patients while encouraging
responsible innovation. Regulations should be adaptive, evolving as AI
technology advances, rather than static rules that quickly become
obsolete.
Special attention must be paid to AI systems that operate
autonomously or make high-stakes decisions. These should face more
stringent oversight than AI tools that merely assist human
decision-makers. Regulatory agencies need adequate resources and
expertise to evaluate AI systems effectively, including the ability to
audit algorithms and training data.
Addressing Bias and
Promoting Equity
Combating algorithmic bias requires proactive measures throughout the
AI development lifecycle. Training datasets must be diverse and
representative, with explicit efforts to include underrepresented
populations. Algorithms should be regularly audited for bias, with
results made public to enable accountability. When bias is detected,
systems should be retrained or retired rather than deployed with known
limitations.
Healthcare institutions deploying AI must monitor outcomes across
demographic groups to detect disparities early. Resources should be
directed toward ensuring that AI benefits reach underserved communities
rather than widening existing gaps. This may require subsidies,
infrastructure investments, and targeted deployment strategies that
prioritize equity over profit.
Protecting Privacy and
Security
Robust data protection measures must be non-negotiable. This includes
strong encryption, strict access controls, and data minimization
principles that limit collection to what’s truly necessary. Privacy
frameworks should give patients meaningful control over their health
data, including the right to know how it’s used and the ability to
revoke consent.
Security standards for healthcare AI systems should be rigorous, with
regular audits and penetration testing. Breach notification requirements
should be strengthened, and penalties for negligent data handling should
be substantial enough to incentivize proper security practices.
International agreements on health data sharing should balance research
needs with privacy protection.
Investing in Human Capital
Rather than viewing AI as a replacement for healthcare workers, we
should invest in training that enables professionals to work effectively
alongside AI systems. Medical education should incorporate AI literacy,
teaching future clinicians how to interpret AI recommendations
critically and when to override them. Continuing education programs
should help current practitioners adapt to AI-augmented practice.
Support should be provided for workers whose roles are disrupted by
AI, including retraining programs and transition assistance. Healthcare
systems should be designed to leverage AI’s efficiency gains to improve
working conditions and reduce burnout rather than simply cutting costs
through workforce reductions.
Fostering Collaborative
Innovation
The development of healthcare AI should involve diverse
stakeholders—clinicians, patients, ethicists, regulators, and
technologists—working together from the earliest stages. Patient
advocacy groups should have meaningful input into AI development
priorities and deployment decisions. Clinical validation should be
rigorous and transparent, with results published regardless of
outcome.
Open science principles should guide AI research, with algorithms and
datasets shared when possible to enable independent validation and
improvement. Public funding should support AI development that addresses
unmet medical needs rather than just profitable applications.
International collaboration should focus on ensuring that AI benefits
global health rather than widening disparities between nations.
Conclusion: Embracing
Complexity
The future of AI in healthcare is neither utopian nor dystopian—it is
complex, contingent, and still being written. The technology offers
genuine opportunities to improve health outcomes, increase efficiency,
and extend quality care to more people. But these benefits are not
automatic or inevitable. They depend on choices we make today about how
to develop, regulate, and deploy AI systems.
We must resist both the temptation to embrace AI uncritically and the
impulse to reject it entirely. Instead, we need sustained engagement
with the technology’s complexities, honest acknowledgment of its
limitations and risks, and commitment to ensuring that it serves human
flourishing rather than narrow commercial interests.
The healthcare AI revolution will succeed or fail based not on the
sophistication of algorithms but on the wisdom of the humans who create
and govern them. By centering patient welfare, prioritizing equity,
demanding transparency, and maintaining human judgment at the heart of
medical care, we can harness AI’s transformative potential while
protecting against its risks.
The future of healthcare is being built now, in research
laboratories, hospital systems, regulatory agencies, and policy debates
around the world. The decisions we make in this pivotal moment will
shape medicine for generations to come. We must choose wisely, guided by
evidence, ethics, and an unwavering commitment to the fundamental
principle that healthcare exists to serve human health and dignity.
As we stand at this crossroads, one thing is clear: the question is
not whether AI will transform healthcare, but how—and whether that
transformation will make medicine more humane, equitable, and effective,
or less so. The answer lies in our hands.
This article explores the multifaceted impact of artificial
intelligence on healthcare, examining both the transformative potential
and significant challenges that accompany this technological revolution.
As AI continues to evolve, ongoing dialogue among all stakeholders will
be essential to ensuring that innovation serves the broader goals of
health equity and human welfare.